Let’s talk about ultrasound imaging in acute muscle injury
We had a small zoom meeting recently to start a conversation about muscle injury. This was an opportunity to share with referrers and other interested people our current interpretation of what the literature is telling us regarding the role of ultrasound imaging in the diagnosis and rehabilitation of acute muscle tears. There were three initial focus points we wanted to share:
1. When is the ideal time to send for imaging?
At 48-hours, imaging will show
· tear versus no tear
· and/or degree of injury
This early evaluation allows for good timely decision for the individual.
A 7-10-day follow-up allows evaluation of the effectiveness of acute management, and confirmation or adjustment of the initial image findings. This is an important step in the determination of likely prognosis.
Later monitoring is based on the individual patient and injury factors for each case as well as determining healing stages and response to treatment, the intersection of each factor contributing to decision making regarding return to play.
2. What is a tear, and how will understanding it affect management?
a. The Cut Analogy
We think acute muscle tears are like getting a cut, except it is one that you cannot see. When you get cut you want to take a good look:
• What’s damaged?
• How bad is it?
• Is that bone I see there?
• I think I am going to need stitches!
The best case scenario is stop the bleeding, bring the edges of the cut together, and hopefully a band aid will do the trick.
A tear of a muscle and/or associated structures is similar. We can still look, and evaluate what’s torn, how bad the tear is, and what the treatment will likely entail.
b. How will it change my management?
Knowing more about any injury allows us to make informed decisions about how we manage our patients:
• Accurate diagnosis leads to appropriate treatment.
• Knowing the extent of injury and monitoring healing will lead to best return to activity timeframes for the individual.
• Knowing what injuries are possible will lead to better treatment decisions.
c. What about VOMIT (victim of imaging technology)?
Everybody has been the recipient of a report with a shopping list of findings, with no clear weighting pointing to a hierarchy of importance within the findings. We believe we have a job to do to contribute to clearer, collaborative reporting. In order to have the best chance of a clear report, we suggest:
• Imaging findings in the acute stage are more easily related to symptoms.
- Send your patients as soon as you possibly can, don’t wait and see if the symptoms resolve first. Knowing that you were right and it was only a minor injury or no injury at all is worth knowing early.
- Injuries of any severity, whether trivial or severe, are much more difficult to relate to symptoms when distant from the initial injury
• Us being clear in our report about what we know & what we don’t know, whether we know source or cause of a finding, one, both or neither, allows for easier and appropriate interpretation of results.
• Know who performs the ultrasound examination, give them a good patient and injury history, and ask a good clinical question; develop a management partnership.
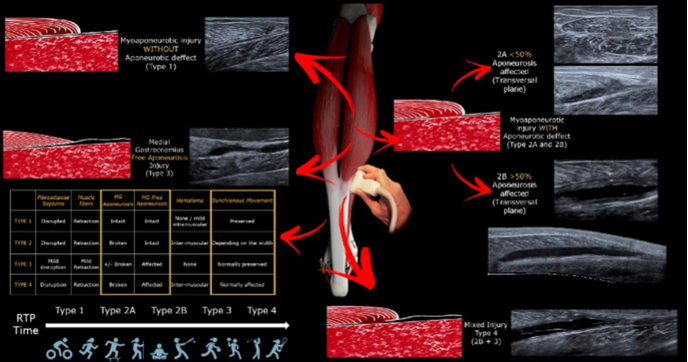
3. We propose… Not reporting grading!
Grading is too simple (because it should be a classification)
For example:
Grading too complex (because it’s a classification)
Grading: there are too many
• Here’s another system of injury classification:
• For every muscle, its own injury classification system? If I’m not confused now, at some point I will be
For now, we’ll be reporting acute muscle injury based on injury characteristics
1. i) No tear; ii) Muscle change (inconclusive), iii) Tear
2. Size of tear; i) linear dimensions, ii) % muscle width, iii) % cross sectional area
3. Structure torn; i) muscle fibres, ii) muscle & tendon structures, iii) complex
4. Site of tear; i) myofascial, ii) musculotendinous junction, iii) complex
5. Haemorrhage; i) dimensions & volume, ii) risk of further haemorrhage
6. Muscle dynamic contraction; i) absent, ii) delayed, iii) present
7. Vascularity at tear site; i) absent, ii) present
As interesting as our recent fracture posts have been, we think the muscle tear story needs to be discussed. Seeing patients early following a suspected muscle injury combined with early follow-up examination, ensures a diagnosis which is accurate and clearly defined as possible to plan for correct and individualized return to activity.